Allergy, Asthma & Clinical Immunology
Case report – Open Access
Min Song, Shan Cai, Hong Luo, Yi Jiang, Min Yang, Yan Zhang, Hong Peng & Ping Chen
Allergy, Asthma & Clinical Immunology volume 15, Article number: 48 (2019)
Abstract
Background
Asthma is often accompanied by peripheral eosinophilia and eosinophilic airway inflammation. This article explores the relationship between asthma and short-term pulmonary infiltrate with eosinophilia, which results from irregular asthma treatment.
Case presentation
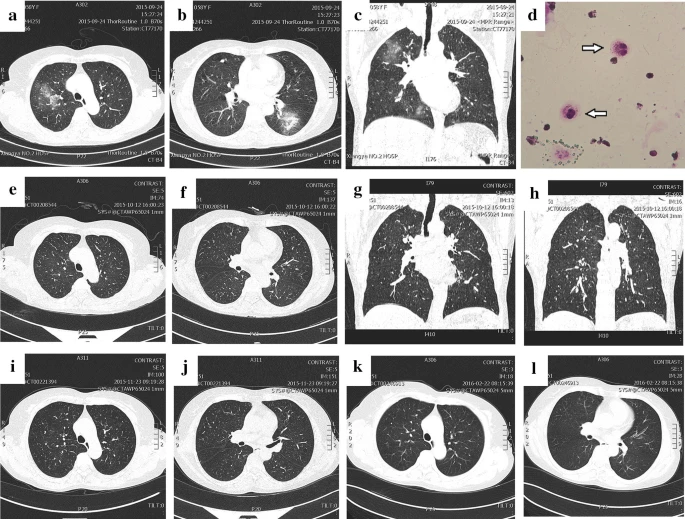
We report five unique cases of asthma-induced short-term eosinophilic pneumonia encountered at our pulmonary and critical care centre in Hunan, China, from January 1, 2014, to August 31, 2018. The 5 asthma patients were women with persistent dyspnoea symptoms, an increased peripheral eosinophil count and a high level of exhaled nitric oxide (FeNO). Chest CT revealed multiple infiltrates and ground-glass opacities in both lung fields in all 5 patients. Four of the 5 patients had increased eosinophils in bronchoalveolar lavage (BAL). Three were positive for reversibility in lung function testing, and two had eosinophil infiltration as revealed by lung biopsy. No antibiotic treatment was given, and after a short period of glucocorticoid therapy and inhaled corticosteroid plus long-acting β2-agonist (ICS + LABA) treatment, the symptoms of all of the patients disappeared. In addition, their blood eosinophils returned to normal, and their lung lesions were quickly absorbed and improved.
Conclusion
These cases show a unique association between short-term eosinophilic pneumonia and asthma. The occurrence of eosinophilic pneumonia can prove fatal during a serious asthma attack. Additionally, the presence of peripheral eosinophilia with lung infiltrates poses a diagnostic challenge for clinicians by creating suspicion of pulmonary infiltrate with eosinophilia when present in asthmatic patients.
