Research, Open Access
Hossein Esmaeilzadeh, Fatemeh Nouri, Seyed Hesamodin Nabavizadeh, Soheila Alyasin & Negar Mortazavi
Allergy, Asthma & Clinical Immunology volume 17, Article number: 16 (2021)
Abstract
Objective
Asthma is one of the most common diseases amongst children. Blood eosinophil count and neutrophil–lymphocyte ratio (NLR) are known as markers for phenotyping asthma. This study was performed to investigate blood eosinophil count and NLR as predictors of hospitalization in pediatric asthma exacerbations.
Data sources and study selections
In this cross-sectional study, children admitted to hospital ward for more severe asthma exacerbation were compared with non-hospitalized children with moderate to severe asthma exacerbation whose asthma exacerbation was managed in emergency department or outpatient clinic. We investigated patients’ characteristic and factors associated with hospitalization.
Results
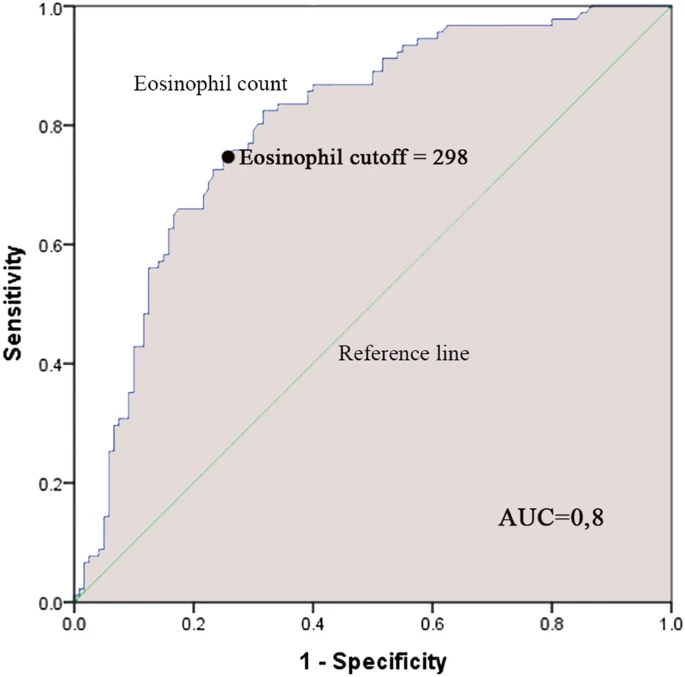
A total of 211 children with moderate to severe asthma exacerbation (mean age 5.76±3.285.76±3.28 years old) were enrolled in the study including 91 hospitalized patients and 120 non-hospitalized patients. For the prediction of hospitalization, an ROC Curve analysis was performed and revealed a cut-off of 298 cells/µL and 2.52 of blood eosinophil count and NLR, respectively. In multivariate analysis, not using an asthma action plan (OR 2.22, 95% CI 1.09–4.49; P = 0.027), a blood eosinophil count ≥≥ 298 (OR 8.79, 95% CI 4.44–17.4; P < 0.001) and an NLR ≥≥ 2.52 (OR 2.13, 95% CI 1.09–4.14; P = 0.027) were associated with hospitalization.
Conclusion
Blood eosinophil count and NLR were found to be higher in hospitalized children with more severe asthma exacerbation compared to non-hospitalized patients. These markers can be indicators for asthma exacerbation severity.
