Respiratory Research Research OPEN
Jack Yang, Ivan Ramirez Moral, Cornelis van ’t Veer, Alex F. de Vos, Regina de Beer, Joris J. T. H. Roelofs, B. Paul Morgan & Tom van der Poll
Abstract
Background
Complement factor C5 can either aggravate or attenuate the T-helper type 2 (TH2) immune response and airway hyperresponsiveness (AHR) in murine models of allergic asthma. The effect of C5 during the effector phase of allergen-induced asthma is ill-defined.
Objectives
We aimed to determine the effect of C5 blockade during the effector phase on the pulmonary TH2 response and AHR in a house dust mite (HDM) driven murine asthma model.
Methods
BALB/c mice were sensitized and challenged repeatedly with HDM via the airways to induce allergic lung inflammation. Sensitized mice received twice weekly injections with a blocking anti-C5 or control antibody 24 h before the first challenge.
Results
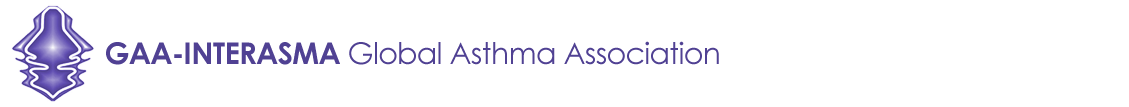
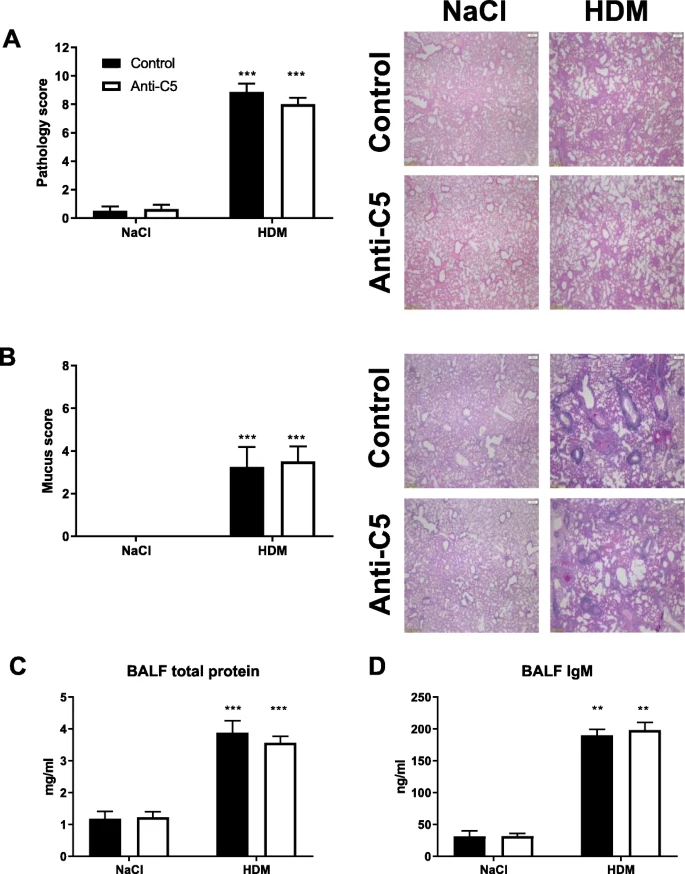
 HDM challenge in sensitized mice resulted in elevated C5a levels in bronchoalveolar lavage fluid. Anti-C5 administered to sensitized mice prior to the first HDM challenge prevented this rise in C5a, but did not influence the influx of eosinophils or neutrophils. While anti-C5 did not impact the recruitment of CD4 T cells upon HDM challenge, it reduced the proportion of TH2 cells recruited to the airways, attenuated IL-4 release by regional lymph nodes restimulated with HDM ex vivo and mitigated the plasma IgE response. Anti-C5 did not affect innate lymphoid cell (ILC) proliferation or group 2 ILC (ILC2) differentiation. Anti-C5 attenuated HDM induced AHR in the absence of an effect on lung histopathology, mucus production or vascular leak.
HDM challenge in sensitized mice resulted in elevated C5a levels in bronchoalveolar lavage fluid. Anti-C5 administered to sensitized mice prior to the first HDM challenge prevented this rise in C5a, but did not influence the influx of eosinophils or neutrophils. While anti-C5 did not impact the recruitment of CD4 T cells upon HDM challenge, it reduced the proportion of TH2 cells recruited to the airways, attenuated IL-4 release by regional lymph nodes restimulated with HDM ex vivo and mitigated the plasma IgE response. Anti-C5 did not affect innate lymphoid cell (ILC) proliferation or group 2 ILC (ILC2) differentiation. Anti-C5 attenuated HDM induced AHR in the absence of an effect on lung histopathology, mucus production or vascular leak.
Conclusions
 Generation of C5a during the effector phase of HDM induced allergic lung inflammation contributes to TH2 cell differentiation and AHR without impacting ILC2 cells.
Generation of C5a during the effector phase of HDM induced allergic lung inflammation contributes to TH2 cell differentiation and AHR without impacting ILC2 cells.