- Letter to the Editor
- Open Access
Allison J. Burbank, Stephen A. Schworer, Amika Sood, Martha Almond, Kelly Chason, Nathan Bean, Haibo Zhou & Michelle L. Hernandez
Respiratory Research volume 22, Article number: 309 (2021)
Abstract
Background
Preclinical studies implicate interleukin (IL)-1β as a key mediator of asthma and have shown the efficacy of IL-1 antagonism for treatment of allergic airway inflammation; human studies in this area are lacking.
Objectives
Our aim was to study the relationship of airway IL-1β to features of acute allergen-induced asthma exacerbation in humans.
Methods
Dust mite-allergic adults with mild asthma underwent inhalation challenge with Dermatophagoides farinae. Fractional exhaled nitric oxide (FeNO), induced sputum and peripheral blood samples were obtained pre- and 24 h post-challenge. Spirometry was performed before and throughout the challenge at 10-min intervals, and allergen responsiveness was defined by a 20% fall in Forced Expiratory Volume in 1 s (FEV1). Sputum samples were analyzed for inflammatory cells, cytokines and chemokines. Multiple linear regression was employed to test the association between sputum IL-1β concentration and biomarkers of T helper type 2 (T2)-dominant inflammation.
Results
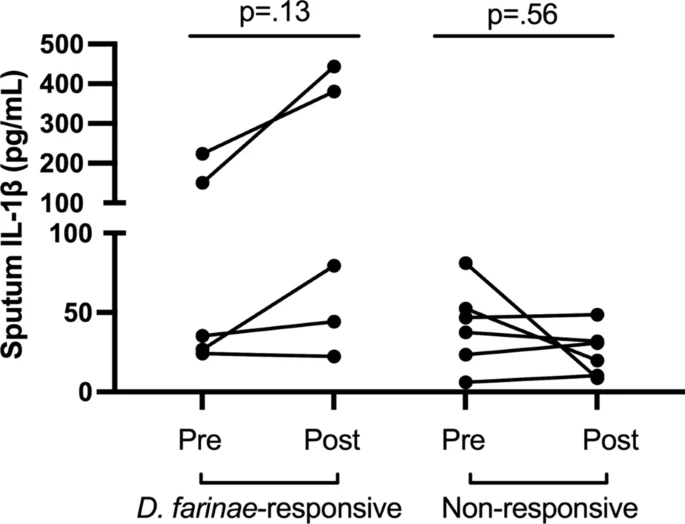
Fourteen volunteers underwent inhaled allergen challenge. Allergen responsive volunteers showed a greater positive change in IL-1β in sputum following allergen challenge compared to non-responders. Higher pre-challenge sputum IL-1β was associated with greater increase in sputum IL-5 (p = 0.004), sputum eosinophils (p = 0.001) and blood IL-5 (p = 0.003) following allergen challenge. Allergen-induced sputum IL-1β production was significantly associated with sputum and blood IL-5 (p < 0.001 and p = 0.007, respectively), sputum IL-4 (p = 0.001), IL-13 (p = 0.026), eosinophils (p = 0.008) and FeNO (p = 0.03).
Conclusions
The positive association between production of IL-1β and biomarkers of T2 inflammation, particularly IL-5, in humans is consistent with work in animal models that demonstrates a link between IL-1β and the pathophysiology of allergic asthma. The role of IL-1β in human asthma warrants further study.
