Biener, L., Frisch, B.C., Skowasch, D. et al. BMC Pulm Med 24, 509 (2024). https://doi.org/10.1186/s12890-024-03322-0
Abstract
Objective
Asthma is linked to atherosclerosis, yet the underlying mediators remain elusive. Eosinophils may contribute to both asthmatic and atherosclerotic inflammation. Hence, this study aimed to explore the potential associations of eosinophils with artery changes among patients with asthma.
Methods
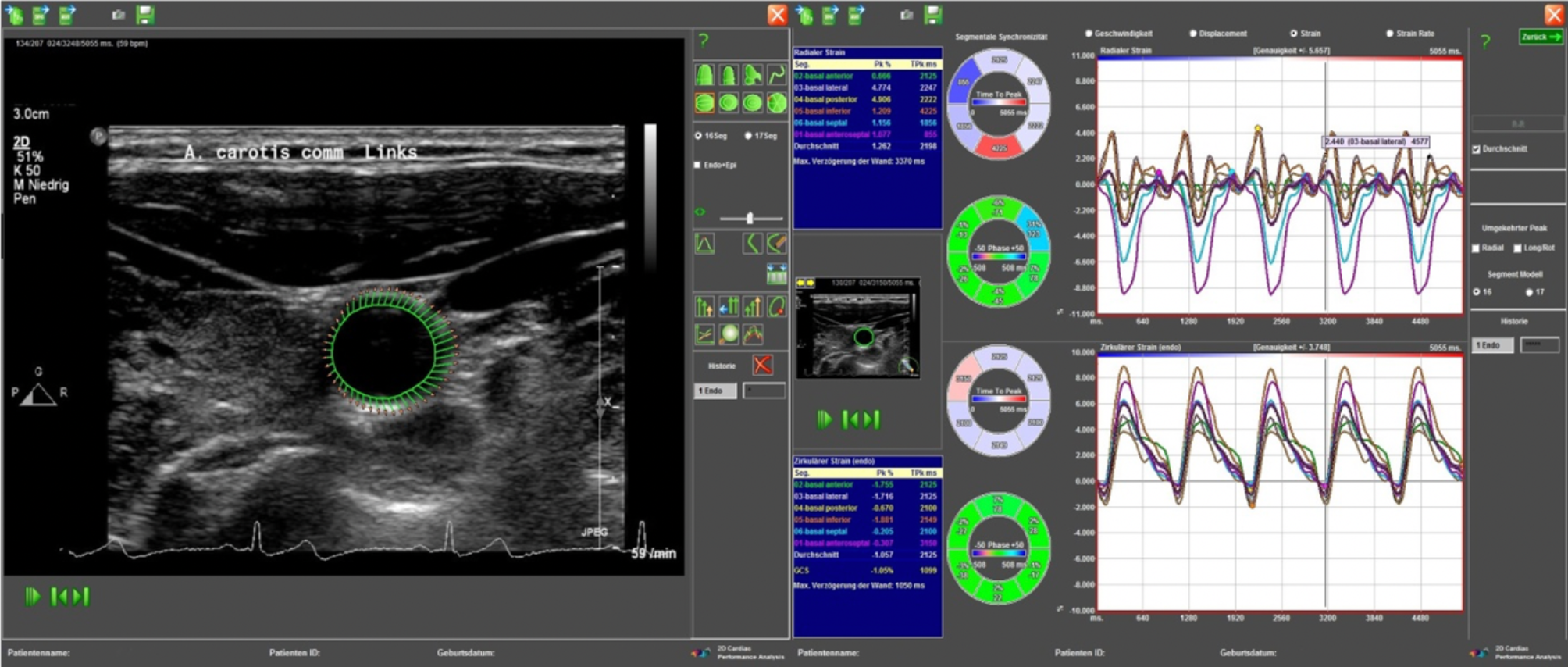
We assessed strain values of the common carotid arteries (CCAs) via vascular speckle tracking and compared asthma patients with low (< 300/µl) and high (≥ 300/µl) blood eosinophil counts (BEC).
Results
We enrolled 100 patients, 42 with a BEC of < 300 and 58 with a BEC of ≥ 300 n/µl. Patients with high BEC exhibited more severe disease, characterized, e.g., by a higher frequency of acute exacerbations (1.3 ± 2.1 vs. 2.6 ± 2.4 n/year, p = 0.005). Both groups presented similar profiles in terms of conventional cardiovascular risk. The high BEC group demonstrated elevated arterial stiffness, reflected by reduced radial strain (mean radial strain of the right CCA: 2.7 ± 1.4% for BEC ≥ 300 n/µl vs. 3.5 ± 1.7% for BEC < 300 n/µl, p = 0.008; left CCA: 2.6 ± 1.4% vs. 4.1 ± 2.2%, p < 0.001). A weak yet statistically significant negative correlation was observed between BEC and radial strain for the right CCA (R2 = 0.131, b=-0.001, p = 0.001) and left CCA (R2 = 0.086, b=-0.001, p = 0.015). However, the prevalence of cerebrovascular disease was similar in both groups (31,0% vs. 50,0%, p = 0.057).
Conclusion
We identified a correlation between BEC and vascular stiffness, which supports the hypothesis that eosinophils may promote atherosclerosis.
