
Research – Open access
Ting Mou, Yujiao Wang, Yufen Fu, Yuxin Wang & Guoping Li BMC Pulmonary Medicine volume 24, Article number: 619 (2024)
Abstract
Objective
Currently, there has been no gold standard for diagnosing small airway dysfunction (SAdf). This study aimed to evaluate the correlation between small airway parameters derived from spirometry and oscillometry in hospitalized patients, assessing the potential of oscillometry as an alternative diagnostic tool for SAdf. Additionally, this study explored the inconsistencies and influencing factors related to spirometry and oscillometry in diagnosing SAdf, conducting a preliminary assessment of these factors.
Methods
A retrospective study was conducted involving data collection from patients who underwent both spirometry and oscillometry between June 1, 2022, and September 1, 2023, at Chengdu Third People’s Hospital was conducted. Initially, 1,771 patients were considered, with 1,446 meeting the inclusion and exclusion criteria. The clinical characteristics and correlations between small airway parameters from the two methods were analyzed based on different lung function data groups. Besides, this study explored the inconsistency between the two pulmonary function tests in diagnosing SAdf in hospitalized patients. Multivariate logistic regression was employed to investigate the factors contributing to these inconsistencies.
Results
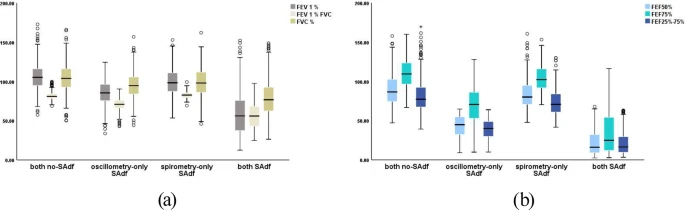
Significant correlations were identified between parameters (reactance area [AX], resonant frequency [Fres], reactance at 5 Hz [X5], difference between resistance at 5 Hz and R20 [R5-R20]) and the forced expiratory flow (FEF) metrics (FEF25%-75%, FEF50%, and FEF75%). Among these, AX showed the strongest correlation, regardless of the severity of forced vital capacity (FVC), forced expiratory volume in one second (FEV1), and the FEV1/FVC ratio. Diagnostic inconsistencies were influenced by factors such as sex, body mass index (BMI), and sputum production. Females, individuals with a high BMI, and those with less sputum were linked to oscillometry-only SAdf, while males, individuals with alow BMI, and those with more sputum were linked to spirometry-only SAdf.
Conclusion
In hospitalized patients, oscillometry could serve as an effective alternative or complement to spirometry for diagnosing SAdf. A greater degree of lung function impairment was correlated with small airway parameters between the two tests. The oscillometry might detect SAdf more sensitively in patients with normal pulmonary function as measured by spirometry. Ultimately, we recommend the combined use of spirometry and oscillometry in hospitalized patients based on its comprehensive assessment of small airway function and potential in timely intervention.
